What Is Hyperparathyroidism?
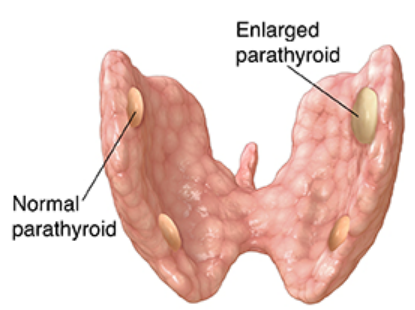
Hyperparathyroidism occurs when the parathyroid glands make too much parathyroid hormone (PTH). The parathyroid glands are four pea-sized endocrine glands located in your neck, near or attached to the back of your thyroid. Endocrine glands secrete hormones necessary for the normal functioning of the body.
Despite having similar names and being adjacent in your neck, the parathyroid glands and the thyroid are very different organs. PTH helps regulate the levels of calcium, vitamin D, and phosphorus in your bones and blood.
Some people with this condition don’t experience any symptoms and don’t need treatment. Others have mild or severe symptoms that might require surgery.
What Are the Causes of Hyperparathyroidism?
In hyperparathyroidism, one or more of your parathyroid glands becomes overactive and makes excess PTH. This could be due to a tumor, gland enlargement, or other structural problems of the parathyroid glands. When your calcium levels are too low, your parathyroid glands respond by increasing the production of PTH. This causes your kidneys and intestines to absorb a larger amount of calcium. It also removes more calcium from your bones. PTH production returns to normal when your calcium level goes up again.
What Are the Types of Hyperparathyroidism?
There are three types of hyperparathyroidism: primary, secondary, and tertiary.
Primary Hyperparathyroidism This type occurs when you have a problem with at least one of your parathyroid glands. Common causes of parathyroid problems include benign growths on the gland and enlargement of at least two glands. In rare cases, a cancerous tumor causes this condition. An increased risk of developing primary hyperparathyroidism also occurs in people who:
- have certain inherited disorders that affect several glands throughout the body, such as multiple endocrine neoplasia
- have a long history of calcium and vitamin D deficiencies
- have been exposed to radiation from cancer treatment
have taken a drug called lithium, which mainly treats bipolar disorder
Secondary Hyperparathyroidism This type occurs when you have an underlying condition that causes your calcium levels to be abnormally low. Most cases of secondary hyperparathyroidism are due to chronic kidney failure that results in low vitamin D and calcium levels.
Tertiary Hyperparathyroidism This type occurs when your parathyroid glands keep making too much PTH after your calcium levels return to normal. This type usually occurs in people with kidney problems.
What Are the Symptoms of Hyperparathyroidism?
Symptoms can vary from mild to severe, depending on your type of hyperparathyroidism.
Primary Hyperparathyroidism Some patients don’t have any symptoms. If you do have symptoms, they can range from mild to severe.
Milder symptoms may include:
- fatigue
- weakness
- depression
- body aches
More severe symptoms can include:
- appetite loss
- constipation
- vomiting
- nausea
- excessive thirst
- increased urination
- confusion
- memory problems
- kidney stones
Secondary Hyperparathyroidism With this type, you may have skeletal abnormalities, such as fractures, swollen joints, and bone deformities. Other symptoms depend on the underlying cause, such as chronic kidney failure or severe vitamin D deficiency.
How Is Hyperparathyroidism Diagnosed?
Your primary care provider might suspect that you have hyperparathyroidism if routine blood tests show high levels of calcium in your blood. To confirm this diagnosis, your primary care provider will need to perform other tests.
Blood Tests Additional blood tests can help your primary care provider make a more accurate diagnosis. Your primary care provider will check your blood for high PTH levels, high alkaline phosphatase levels, and low levels of phosphorus.
Urine Tests A urine test can help your primary care provider determine how severe your condition is and whether kidney problems are the cause. Your primary care provider will check your urine to see how much calcium it contains.
Kidney Tests Your primary care provider might take X-rays of your abdomen to check for kidney abnormalities.
What Are the Treatments for Hyperparathyroidism?
Primary Hyperparathyroidism
You might not need treatment if your kidneys are working fine, if your calcium levels are only slightly high, or if your bone density is normal. In this case, your primary care provider might monitor your condition once a year and check your blood-calcium levels twice a year.
Your primary care provider will also recommend watching how much calcium and vitamin D you get in your diet. You’ll also need to drink plenty of water to reduce your risk of kidney stones. You should get regular exercise to strengthen your bones.
If treatment is necessary, surgery is the commonly used treatment. Surgical procedures involve removing enlarged parathyroid glands or tumors on the glands. Complications are rare and include damaged vocal cord nerves and long-term, low levels of calcium.
Calcimimetics, which act like calcium in the blood, are another treatment. These drugs can trick your glands into making less PTH. Primary care providers prescribe these in some cases if surgery is unsuccessful or not an option.
Bisphophonates, which keep your bones from losing calcium, can help reduce the risk of osteoporosis.
Hormone replacement therapy can help bones hold on to calcium. This therapy can treat postmenopausal women with osteoporosis, although there are risks involved with prolonged use. These include an increased risk of some cancers and cardiovascular disease.
Secondary Hyperparathyroidism
Treatment involves bringing your PTH level back to normal by treating the underlying cause. Methods of treatment include taking prescription vitamin D for severe deficiencies and calcium and vitamin D for chronic kidney failure. You might also need medication and dialysis if you have chronic kidney failure.
What Are the Complications Associated with Hyperparathyroidism?
If you suffer from hyperparathyroidism, you might also have a condition called osteoporosis which is also sometimes referred to as “thinning” of the bone. Common symptoms include bone fractures and height loss due to vertebral body (spinal column) fractures. This can develop when excess PTH production causes too much calcium loss in your bones, making them weak. Osteoporosis typically occurs when you have too much calcium in your blood and not enough calcium in your bones for a prolonged period.
Osteoporosis puts you at a higher risk for bone fractures. Your primary care provider can check for signs of osteoporosis by taking bone X-rays or doing a bone mineral density test. This test measures calcium and bone mineral levels using special X-ray devices.
What Is the Long-Term Outlook?
According to the Cleveland Clinic, surgery can cure most cases of hyperparathyroidism. If you and your primary care provider opted to monitor your condition rather than treating it, making several healthy lifestyle choices can help you fight symptoms. Drink plenty of water, and get regular exercise. You should also monitor the amount of calcium and vitamin D you consume.